The expedition of pain started for me the evening of Monday, February 18th. Around 5 P.M. I was running home from work and had just a touch of indigestion. Nothing unusual, just a little stomach upset. Amy and I had a normal dinner and a drink and nothing seemed too out of the ordinary, though the indigestion was still there. We were in bed around 10 and I slept soundly until 11, when I woke up with noticeably more discomfort. At this point it felt like food poisoning, and I kept expecting the usual 'passing' of waste, but nothing was happening. I was up and down from bed several times and was even browsing on my phone for symptoms of appendicitis, since what I had now seemed similar to what Amy suffered through with that several years ago. By 2 A.M. I'd had enough and woke Amy.
She drove me down to what was an empty emergency room at Fairview Riverside. It was an uncomfortable ride, but I was still in control of myself and managed to walk in and start getting checked out. I was here for three hours with an IV in my arm and some mild pain medications that seemed to be doing the trick. Over this time I had a CT scan and and ultrasound, neither of which showed my appendix nor the torsion in my intestine. This coupled with the location of my pain, in the area just below my navel, and the fact that I had had bowel movements during the previous day led the doctors to feel that it was probably just a bad stomach virus and I was sent home with a bottle of hydrocodone, a pretty solid pain pill. I was actually a little relived that it was just a bug, and I could get back to things in a few days. Some home we went, me to the couch and Amy to bed, so she could get some rest and I could toss and turn.
I didn't get a lot of rest, and around 10 A.M. Wednesday morning, I was nauseous and having massive stomach cramps. I soon started having massive heaves, throwing up everything I'd eaten in the last half a day, and hard enough that I had a bloody nose. I was curled up on the floor moaning and crying out for Amy and eventually worked my way over to the other side of the house where she could hear me. There was absolutely no question we'd be going back to the ER. So, around 11AM we were back at Fairview Riverside.
I was soon changed and back on a table, this time on my left side, since it was the only position I was remotely comfortable, and with an IV back in giving me .4MG/hour of some kind of narcotic (I sure remember those numbers). Around here I really lost track of time as the pain increased. I'm not sure how long I was in the ER, but I had one long episode of throwing up while talking to the doctor. While they double checked the CT scan and still didn't see anything they were concerned enough to want me to stay for a while. So an ambulance transport was arranged for me to be moved over to University of Minnesota Medical Center on the East bank for observation. I had it together enough to get off the bed and onto the gurney myself since it was only a few feet. Amy was left to drive herself over. I can only imagine what she was going through at this point.
As I was in my new room at UMMC I didn't look at anything other than the wall. Occasionally someone would come in and want to palpate my stomach, often enough that I was getting pissed off. Yes the pain was still there, no it hadn't moved, why don't you talk to the last person that did this. One doctor even put me through that several times. Part of the problem was that each time I rolled from my side to my back, then to my side again, it took many minutes for the pain to squelch enough that it was tolerable. The plan, as I understood it, was to take blood from me again in the morning (since they already had for my second ER visit) and if there were still problems have a surgical consult somewhere around 6AM.
The only problem for me is the pain meds were no longer doing anything, and I was beginning to moan and groan non-stop, occasionally yelling, except for the times where I'd pass out for a few minutes. They have a 0 to 10 pain scale you are supposed to rate your pain on and I repeatedly was saying 9, 9, 9. I remember quite vividly regularly clawing at the air just trying to grasp at something and sometimes staring in terror into Amy's eyes and begging her to make it stop. This went on for a long time, but I can't really say the exact time since it was basically a black pit for me. Sometime during the evening nurse Andrew came on duty and started going to bat for me. He gave me a some extra checks to see if it was simply bad constipation (if only) and got my pain meds bumped up to 1mg/hr. Sadly even at that level it wasn't doing anything.
He eventually got the powers that be to get a surgical consult in immediately since the medication and other obvious checks weren't doing anything, and my pain kept increasing. Clearly, he said, there is something really wrong with this guy. Amy had been telling them that I handle pain really well, and if I'm screaming then it has to be really bad.
So it was, around 2AM, the anesthesiologist came up to my room to help get me prepped to move and I was soon being wheeled down to the OR. I didn't really care what they did, I just wanted to be put under. Amy and I waited outside the OR while she held my hand and I wailed on, the only relief being that I knew I'd soon be unconscious. The plan was that they would do an exploratory laproscopic surgery (insert a camera and have a look around) then deal with whatever it was when they came to it. I asked Amy to call my parents when I went in. The surgeon, Dr. Harmon, came over and introduced himself putting a gentle hand on me, and I was soon wheeled off into the OR.
They had me roll onto my back, then transferred me from the cot to the operating table and strapped my arms down and put a mask on my face. The last thing I said to them was that I had a really low resting pulse and I'd probably set off their alarms (as I had been all day). Then I was out.
Some time later I groggily came to in a recovery room, with a nurse attending to me. I pretty much had no idea what had happened, but she chatted to me and let me know where I was and that my parents and Amy were waiting for me. After she made sure I was coming around OK, I was wheeled up to a recovery room, which is where I first saw Amy and my parents from inside my fog. A few nurses moved me to my bed and got me hooked up to all kinds of devices, and we all sat and stared at each-other. And like it had started, Amy holding my hand.
I later learned that I had cecal volvulus, which they found pretty quickly with the laproscopy. Unfortunately the only way to deal with this was to open me up with a 10 inch incision starting about 1 inch above my navel and going downwards. Then removing about 5cm of small intestine, the cecal valve, and the vertical section of my large intestine, for about a foot total. That includes my appendix as well. Full recovery, 6-8 weeks. Right now, my stomach is tender and sore, but nowhere near the pain I had been feeling.
.png) |
| What it looked like before. The purple blob is the choked off small intestine. Courtesy of www.stanford.edu. |
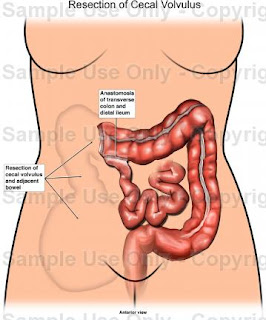 |
| The after, with the cecal valve and ascending lower intestine removed. Courtesy of eyewitnessanimations.medicalillustration.com |